Red blood cells grown from the laboratory are underway in the UK as part of the world's first trial of conduction blood transfusion using fresh blood cells extracted from blood stem cells of a human adult donor. The trial aims to treat people with blood disorders and patients in need of blood transfusions, which are not always available in medical facilities.
Lab-Grown Red Blood Cells
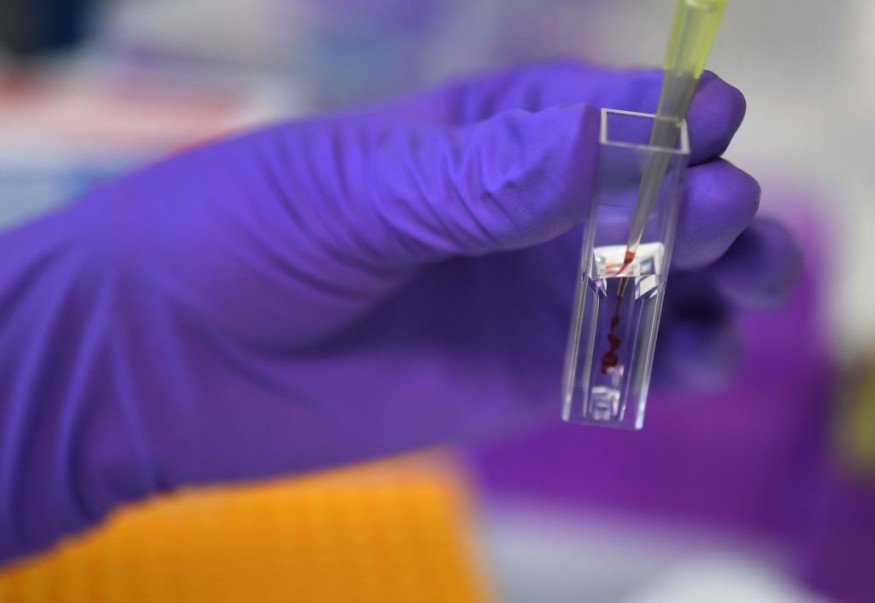
The lab-grown red blood cells were made under the REcovery and survival of STem cell Originated REd (RESTORE) clinical trial funded by the National Institute for Health and Care Research (NIHR). The trial was conducted by researchers from the University of Bristol, which started the first human testing of blood stem cells turned into red blood cells in the laboratory.
The RESTORE clinical trial will test how long a small blood transfusion equivalent to 2 teaspoons of the laboratory grown red blood cells will last in the body, compared to the same amount of the natural and standard red blood cells from the same donor.
The researchers already administered the artificial blood to at least two participants of the study, but they acknowledged that further trials are needed.
What are Red Blood Cells?
Red blood cells are known for supplying oxygen all over the body, supporting different organ function and overall health of its host. Under the microscope, these cells appear to be round and flat, similar to the shape of a doughnut with a hole at its center. An individual can check with his or her healthcare prover the state of their red blood cells through a blood test.
According to the University of Rochester Medical Center (URMC), red blood cells have a protein inside them called hemoglobin, which carries oxygen, and they can remove carbon dioxide from our body and bring it to our lungs to exhale. Made in the bone marrow, a red blood cell typically has a lifespan of around 120 days or four months before they die.
In real-world events, there are instances where a person undergoes an accident or other life-threatening medical condition, resulting in loss of red blood cells. In these circumstances, the person will experience iron deficiency or anemia and be required for red blood cell transfusion, generally known as blood transfusion.
What is Blood Transfusion?
Prior to the NIHR-funded clinical trial, the blood transfusion process often gets its source blood from donors or blood banks, which are used during emergency cases or scheduled operations.
According to the Cleveland Clinic, a blood transfusion aims to provide blood or blood components if someone lost blood due to an injury, during a surgery, or have certain medical conditions, as mentioned earlier in this article.
Blood components include cryoprecipitate and platelets which helps our blood clot. In addition, it also contains plasma which carries nutrients our body needs. Lastly, red blood cells are also a component of the blood, as emphasized before.
Types of Blood Disorders
In addition to anemia, patients may need a blood transfusion if they are suffering from certain cancer types, hemophilia, or the sickle cell disease, the US clinic adds.
The Centers for Disease Control and Prevention (CDC) also highlights some of the types of blood disorders which include the following, in addition to the ones mentioned in the previous section:
- blood clots or venous thromboembolism
- hereditary hemorrhagic telangiectasia (HHT)
- thalassemia
- vitamin K deficiency bleeding
- Von Willebrand disease
- women's blood disorders
Related Article : Dinosaur Red Blood Cells, Collagen Found in Fossils?
© 2025 NatureWorldNews.com All rights reserved. Do not reproduce without permission.





