Scientists were able to convert donated lungs into universal transplant organs. As a result, lungs are now theoretically applicable to be used by any patient who needs a lung transplant during emergency cases.
The unique development of this new study is that the converted lungs can also be used regardless of the blood type of the recipient.
The study's researchers used a device to conduct an experiment and allowed the donated lungs to be kept alive outside the human body.
The practical results of the experiment suggest that the lungs can be used by any recipient as long as they are in the right size. The breakthrough discovery can potentially decrease the waiting time of patients who anticipate a lung donor with a similar blood type as theirs.
In the meantime, the researchers are still planning to engage in clinical trials with live human subjects.
Lungs as Universal Transplant Organs
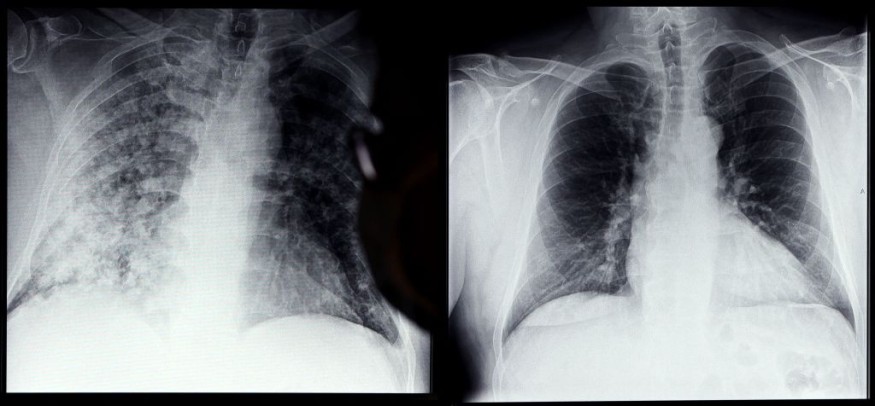
The new study published in the journal Science Translational Medicine on Feb. 16 addressed the challenges surrounding lung transplantation. It has been known that a lung donor with a similar blood type is required for his or her own lungs can be used by other recipients during emergency cases.
Recipients with blood types A, B, and O should receive the same type of blood. However, the new study was able to successfully demonstrate the conversion of lungs as a universal transplant organ by changing the blood type of the particular lung into other types during an experiment
Ex Vivo Lung Perfusion Experiment
The researchers performed experiments known as ex vivo lung perfusion (EVLP), which allowed the lungs to remain alive and function even outside the human body, as per Live Science.
Under the EVLP, the researchers used two enzymes, FpGalNAc deacetylase, and FpGalactosaminidase, to convert the first group of lungs containing blood type A into a new set of lungs with bloody type B. Furthermore, the process was repeated by combining and converting the three blood types.
Antigen has been removed from the blood type A lung group to make the process possible. The yielded results show no changes in the quality and health of the lungs.
Further Study and Clinical Trials on Humans
As per one of the study's authors, Dr. Marcelo Cypel, a surgical director at the Ajmera Transplant Centre and a professor at the University of Toronto, he and his team are planning to conduct experimental tests and clinical trials with human recipients.
The new study's breakthrough discovery is of paramount importance since emergency services in hospitals around the world are often faced with the challenges of lung transplants when the necessity arises that a patient needs a new set of lungs.
According to a 2019 report published in The Journal of Heart and Lung Transplantation, "patients with blood type O have a 20% greater risk of dying while waiting for a lung transplant than those with other blood types," as cited by Live Science.
Similar to a blood transfusion, the biological processes inside the human body during a lung transplant require the same types of blood between the donor and the recipient. If blood types do not match, a human's immune system may have the tendency to attack the unfamiliar donated blood, as per the American Cancer Society.
Related article : Woman Survives 6 Days Without Lungs -- How?
© 2025 NatureWorldNews.com All rights reserved. Do not reproduce without permission.





