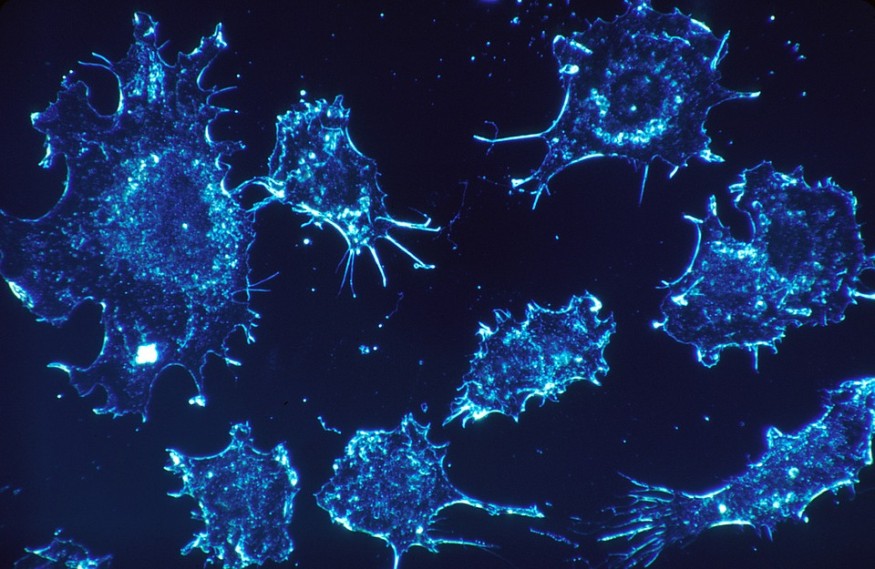
Fungi living in the gut can move into the pancreas, activating cells that could bring cancer, new research revealed.
The researchers, in their study published in Nature, describe how they explored fungal organisms in mice and people with pancreatic cancer.
The group found that specific types of fungal growth can enter the pancreatic channel, which is the tube that the pancreas uses to convey stomach-related juices to the digestive organs.
They additionally discovered that giving mice with the most well-known type of pancreatic cancer growth a reliable antifungal medication could diminish their tumors by up to 40%.
Dr. George Miller, M.D., a hepatobiliary surgeon from New York University Perlmutter Cancer Center and serves as the study's co-author, said in NYU's press release that their group's new investigation is the first to affirm that the fungal population promotes changes too in tumor detection and growth.
Pancreatic Cancer
As indicated by the Centers for Disease Control and Prevention (CDC), pancreatic cancer is among the top 10 common cancers among males and females in the United States. CDC added the occurrence rates have ascended by almost 1.2% every year over the last few decades.
National Cancer Institute (NCI) added that 56,770 individuals in the United States would discover that they have pancreatic cancer in 2019.
NCI added 45,750 patients passed away because of the disease. These figures speak to 3.2% of all new cancer cases and 7.5% of all cancer deaths, respectively.
The organ's strategic location inside the digestive system implies that detecting early signs of pancreatic cancer is challenging. For some individuals, the disease has just advanced when they get the diagnosis, which made it harder to treat.
The NCI additionally estimated that during the years 2009 to 2015, 9.3% of people with pancreatic cancer endure five years or longer after their diagnosis.
There are various kinds of pancreatic cancer, depending upon the tissue type and area of origin. The most widely recognized of these—and the subject of the investigation—is pancreatic ductal adenocarcinoma (PDA), where about 90% of pancreatic cancer growth is located.
Study tracked the progress of fungi from the gut
Dr. Miller and associates, in their study, broke down feces tests from mice with and without PDA. They utilized advanced factual and genomic apparatuses to screen the species and quantities of parasites for more than 30 weeks.
By labeling fluorescent proteins onto the parasites, the group was ready to follow their study from the digestive organs into the pancreas. They found that the malignant and noncancerous murine pancreases contrasted in the size and part of their contagious population. They additionally observed these distinctions in human pancreatic tissue samples.
The most perceptible characteristic was the increase in the species belonging to the Malassezia genus in the cancer tissues.
Other parasitic species, for example, are Parastagonospora, Saccharomyces, and Septoriella, which likewise expanded to a lesser degree.
Co-senior study author Deepak Saxena, Ph.D., a professor in the College of Dentistry at NYU, noted that Malassezia—generally found on the skin and scalp—are responsible for dandruff and some forms of eczema. She added that recent studies have also linked them to the skin and colorectal cancer.
The researchers discovered that treating mice with a reliable antifungal medication called amphotericin B decreased tumor weight by 20 to 40%. The treatment additionally decreased ductal dysplasia, a beginning time in the advancement of pancreatic cancer growth, by 20 to 30%. The researchers noted that antifungal treatment supported the anticancer intensity of gemcitabine, a standard chemotherapy medication, by 15 to 25%.
Malassezia triggers immune mechanism
Further examinations unveiled that pancreatic cancer growth develops 20% quicker when the organ contains Malassezia genus. The specialists found this when they reintroduced these growths into the pancreas in treated mice.
When other basic parasites are available close to Malassezia species, the malignant growth doesn't develop quickly.
The researchers propose that Malassezia raises pancreatic malignant growth chance by setting off an immune instrument.
The immune instrument has a place with an old piece of the immune system that battles the disease. In any case, it can likewise advance cell development after the condition has improved, and the healing stage has started.
Previous examinations have demonstrated that the immune supplement can advance the kind of tissue development that happens in cancer.
© 2025 NatureWorldNews.com All rights reserved. Do not reproduce without permission.





